COVID-19 and the Aging Brain
2020/2021 IOG Report
 By Ana M. Daugherty, Ph.D.
By Ana M. Daugherty, Ph.D.
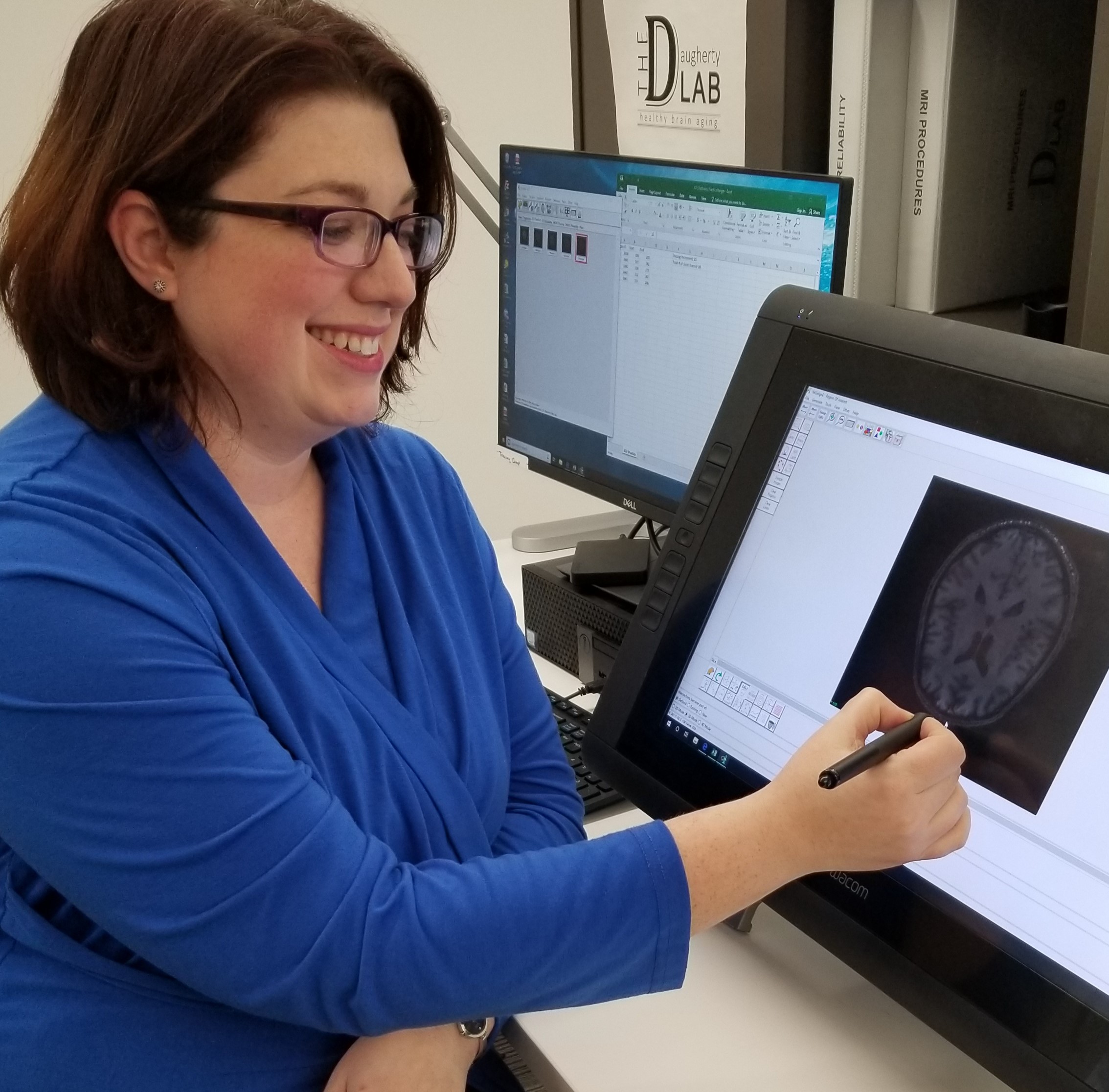
Director of the Healthy Brain Aging Laboratory and Assistant Professor at WSU
Our brains change across the entire lifespan. From childhood to our final years, health factors modify our brain structure and functions. The memory function of a 70-year-old, for example, has been sculpted by health and lifestyle forces that began decades earlier.
This perspective on brain aging inspires hope. We can make small decisions each day to build healthy habits and well-being that help maintain our cognitive function into our latest years. This motivates my research to understand how vascular and metabolic health functions interact with the aging brain and can increase risk for dementia, like Alzheimer's disease. In the Healthy Brain Aging Lab, we partner with community members to follow a participant over time, using MRI, blood measures and lifestyle assessments to characterize the dynamics of health risk and protection in the course of cognitive aging.
In 2020, a new category of risk factors for dementia emerged related to the COVID-19 pandemic. Most people living through this period will consider COVID-19 a benchmark that divides time into pre-COVID and post-COVID. The same is true of my study of aging across the lifespan. In research, we refer to this as a history effect: events outside of a study that affect a study's outcome. In other words, the effects of COVID-19 will echo through my studies for the next several decades.
In my research, I look for connections among vascular and metabolic functions, and it is there that I began to think of COVID-19 as a new risk factor for dementia. I study how inflammation and oxidative damage are parts of healthy cell function, but too much of either contributes to the declines in brain function typical in aging. Poor cardiovascular health worsen these effects to further increase risk for Alzheimer's disease and related dementia. The COVID-19 disease shares similar mechanics to the aging process that I study. The SARS-CoV-2 virus that causes the COVID-19 disease initiates severe inflammation and oxidative stress as part of the typical immune response, and cardiorespiratory symptoms are common. For patients with severe symptoms, COVID-19 may act to accelerate age-related declines in brain structure and function.
In addition to the health risk, we also consider the substantial disruption to daily activities as a loss of protective factors for many older adults during the pandemic. Ample research has shown social interaction and access to community resources promote cognitive resiliency. The community health response to COVID-19 required social distancing, and the isolation and inactivity may also increase dementia risk.
At this time, the possibility of COVID-19 as a risk factor for dementia is only speculation; a hypothesis that requires testing in studies that follow COVID-19 patients over long-term recovery to collect biomarkers of aging, Alzheimer's disease and related dementia. Valuable data will come from on-going studies of aging across the lifespan that allow us to track individual changes from before to after COVID-19, such as the long-term studies that my colleagues and I conduct in Detroit.
The pandemic has been an extreme event that united the global community in our shared distress and our collective resiliency. There is cause for optimism. Borrowing a lesson from a lifespan perspective of aging:
We are the sum of our experiencespositive and negativeand within our ability, we can choose to tilt the scale towards the positive.